Putting healthcare at the heart of communities
Despite the unprecedented levels of global wealth created by economic development over the past century, millions of people across vast regions of our planet are dying unnecessarily through poor healthcare.
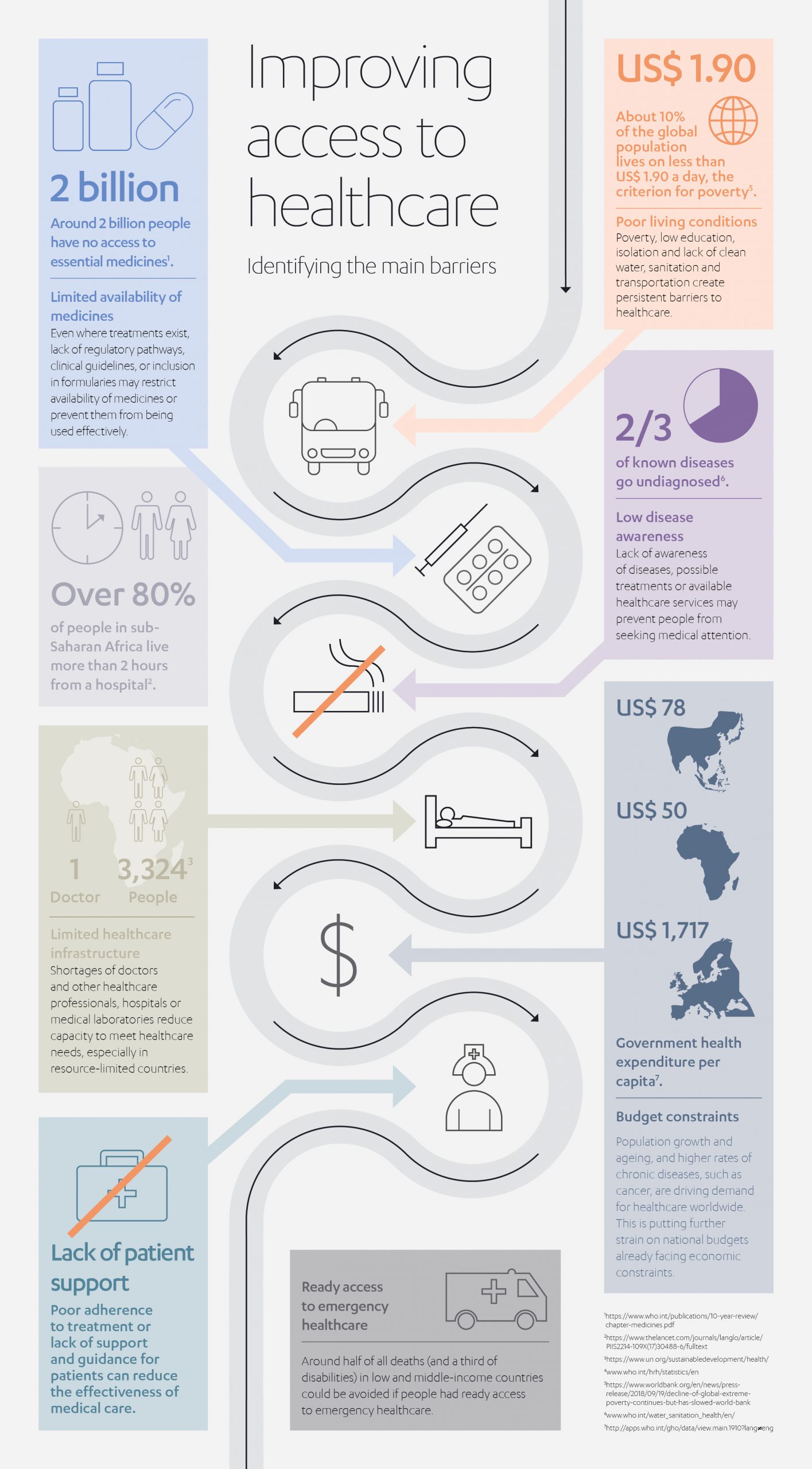
At the heart of this global healthcare challenge is the issue of access – enabling people to obtain the expertise, facilities and treatments they need.
A basic problem is one of geography: many of the most unequal countries in the world are also the largest – where widely dispersed populations live many miles away from their nearest points of primary healthcare.
Two-thirds of sub-Saharan countries, for example, fail the World Health Organization’s (WHO) global target of 80% of people living within two-hours of a hospital.[1] A worrying statistic, given around half of all deaths (and a third of disabilities) in low and middle-income countries could be avoided if people had ready access to emergency healthcare.[2]

But enabling better healthcare access is about much more than how far you live from the nearest healthcare center. Even if a sick or injured person in a low-income country does manage to reach a hospital or healthcare center, they often face a mountain of further problems to access the care they need. Fundamental problems like a shortage of equipment and medicines; long waiting times; variable quality of drugs and medical aids; inadequate information on healthcare choices and poor referrals systems. This is, of course, further compounded by the unattainable cost of care and lack of affordable insurance cover to bridge this gap.
There is an added element to the healthcare conundrum, too. Improving access to healthcare is not only beneficial for the health of individuals, but also for the economic ‘health’ of the countries they live in. In the words of the WHO, better health “makes an important contribution to economic progress, as healthy populations live longer, are more productive, and save more.”[3]
In fact, it has been estimated that the economic performance of developing countries increased significantly with an improvement in public health[4], with GDP growing by 4% for every one year improvement in life expectancy[5].
For over 25 years, the Jameel family has made their its own contribution to improving access to healthcare through the work of the global family philanthropy, Community Jameel.
As far back as 1995, it established the Abdul Latif Jameel Hospital, the first non-profit rehabilitation hospital in Saudi Arabia, and as a participant in the founding of the King Salman Disability Research Center. More recently, Abdul Latif Jameel has established partnerships with medical device innovators and innovation facilitators such as Cyberdyne, Cellspect and JOMMD.
The latest step in its commitment to improving global access to healthcare was unveiled earlier this year, with the establishment of Abdul Latif Jameel Health.

Headed by Akram Bouchenaki, formerly an Executive director with Gilead Sciences, Abdul Latif Jameel Health aims to invest in projects, partners and products to unlock access to affordable high quality healthcare for communities across the developing world, including those Middle East, Africa and South and South East Asia.
In the second of two interviews, we spoke to Akram about the opportunities and objectives for Abdul Latif Jameel Health and his vision for the future.
Where do you see the biggest opportunities for Abdul Latif Jameel Health?
The current pandemic has demonstrated the central importance of healthcare systems, and the need for them to be strong, funded, well organized and well supplied. Personally, I believe this crisis will reorient healthcare policies globally. Particularly in our part of the world, it’s going to be even more critical that policy makers dedicate more resources to strengthen the resilience of public healthcare systems.
In this context, we see Abdul Latif Jameel Health as a key player in facilitating and accelerating supply, and improving accessibility, both at national and at international level.
We are already seeing some governance changes around healthcare policies and healthcare institutions. For example, there are talks about an African Drug Agency to accelerate the approval of novel drugs to African markets.
 The role of the Africa Union is definitely growing. We want to be in a position to facilitate and enable the conversations around healthcare to try and address public health issues, both on communicable diseases and non-communicable diseases, which are a growing problem in emerging markets.
The role of the Africa Union is definitely growing. We want to be in a position to facilitate and enable the conversations around healthcare to try and address public health issues, both on communicable diseases and non-communicable diseases, which are a growing problem in emerging markets.
What kind of involvement might that mean in practice?
The vision is to be an end-to-end provider of healthcare solutions. This could take many forms, depending on the needs of the specific market. It may involve working with labs on developing new drugs, working with governments or NGOs on distributing drugs and getting them out to the market, and ensuring sustainable access to high quality healthcare solutions.
 Let me give you an example. If you look at a disease like hepatitis B or C, it’s common in many parts of the world, yet many people are only diagnosed when it’s too late, when they have liver cancer or advanced cirrhosis,. Hepatitis B, for example, could be easily prevented by vaccinating children at birth; Hepatitis C could be cured if diagnostic tools are made available during medical check-ups or screening campaigns. This is particularly the case in dispersed populations where portable ‘point-of-care-testing’ (POCT) devices make widespread screening a tangible possibility.
Let me give you an example. If you look at a disease like hepatitis B or C, it’s common in many parts of the world, yet many people are only diagnosed when it’s too late, when they have liver cancer or advanced cirrhosis,. Hepatitis B, for example, could be easily prevented by vaccinating children at birth; Hepatitis C could be cured if diagnostic tools are made available during medical check-ups or screening campaigns. This is particularly the case in dispersed populations where portable ‘point-of-care-testing’ (POCT) devices make widespread screening a tangible possibility.
Our aim is to establish ourselves as a provider of cohesive solutions for situations like this. We want to be in a position to make diagnostic tools and POCT more accessible to communities, particularly in more remote or deprived areas, to make it easier, faster and cheaper for people to get tested.
This is one step that is absolutely crucial, irrespective of the disease, whether it be heart disease, diabetes or infectious diseases. And it is an area where we have already made some progress via our partnership with the Japanese company Cellspect, which has developed a state-of-the-art, portable testing tool.
Then comes the treatment phase and the need to get new therapies and products into markets more quickly. Studies show that once a product is approved in Europe or the United States, it can take anywhere between seven to 16 years before it gets to more remote parts of the world. We want to accelerate that by working with regulatory authorities to speed up this process and provide earlier access to medicine.
 Education and awareness are other important issues. There needs to be a joined-up approach to disease awareness programs with healthcare authorities, and healthcare providers so people understand the risks, the symptoms, how diseases occur, how to get tested, and so on.
Education and awareness are other important issues. There needs to be a joined-up approach to disease awareness programs with healthcare authorities, and healthcare providers so people understand the risks, the symptoms, how diseases occur, how to get tested, and so on.
These are some of the situations we see ourselves being involved in, as an end-to-end healthcare solutions provider in our territories.
Which territories will you focus on?
Our plan is to leverage the existing – and growing – footprint of Abdul Latif Jameel and extend it further into those areas with most need, either directly or through partnerships. North Africa is important, but also West Africa, East Africa with countries like Kenya and Tanzania, and South Africa, which is a key market for medicine and healthcare.
The Middle East is another area of focus where many countries have an existing well-funded healthcare system, but there is still a big need for better access to novel, innovative medicines. We want to be an accelerator to bring those medicines and solutions faster into the region. We are also looking at South and South East Asia, which has a diversity of healthcare contexts and a lot of unmet medical needs. So, it’s a fairly wide footprint we are targeting.
How do you hope to address the challenges in such diverse regions?
It’s essential to adopt a tailored approach in each of these markets. In most cases, you will have different patterns of disease, different infection rates, different treatment issues and different access to healthcare. The other big issue is the financial aspect – how is treatment funded in the different countries. All these factors will determine how we adapt our approach; tailoring it to achieve optimal results both for the market and commercially for our partnerships.
Nevertheless, there are some consistent building blocks that will always be at the heart of our proposition.
Firstly, we want to provide, to whatever market, the best possible distribution in terms of quality and reliability. We have to be best-in-class, both to our customers and to our partners who have entrusted us with their assets. Then secondly, we will tap into our local intelligence about the different market conditions, so we can target our offer to the specific needs of the market. As an example, if you look at HIV infection rates, you don’t necessarily address things the same way in countries where you have hundreds of thousands of new infections every year, versus countries where you have a few thousand new infections every year,.
Similarly, with metabolic disorders like diabetes, some countries are witnessing a skyrocketing rate of new cases, but in other countries it is much lower, as it tends to be linked to economic development. That’s the kind of adjustment and alignment we would consider in our approach to the various markets.

What strategies and models will you need to adopt to achieve this?
The key is to understand the specific context of each market. It might be that a country has lack of central diagnostic labs. In that scenario, we might seek to provide point-of-care testing for remote access to diagnostics, enhance communication systems between healthcare providers and patients, and organize the systems and processes for getting people to seek care and seek treatment.
The other aspect is tailoring our offer in terms of the partners we work with. The partnerships we establish locally are crucially important, and they are with the best actors in the field There is no point partnering with an organization to provide a solution that is out of scope for a certain territory. It has to be viable and compatible with the healthcare system in that country so people will really benefit from it. That’s where conversations with healthcare authorities, providers, companies, are going to be vital for us in developing that knowledge and addressing our solutions to the most pressing needs.
At the end of the day, it’s about trust.
People need to trust the health solution you provide to them. And we need to earn that trust in terms of the solutions we provide, the people we work with and the way we do business.
In any healthcare market, there are factors you can’t control, such as cultural or political issues. What difference will this make to your work and what kinds of partners can help you respond to these?
You’re absolutely right! There are many factors, like funding, culture, custom, infrastructure, that affect access to health, but over which we have limited influence. That’s another reason why we really need to understand the local dynamics, adapt to them, identify the most appropriate partners, and provide an offering that is adaptable to the particular context. In terms of partners, it could be NGOs, local healthcare providers, government organizations or healthcare companies.
Abdul Latif Jameel is already an investor in the healthcare sector, with its investments in Cyberdyne, Cellspect and JOMDD, as well as some other initiatives. How do these fit into the Abdul Latif Jameel Health picture?
These examples illustrate the type of operating model we might pursue in particular markets or sectors – taking breakthrough innovations, accelerating their commercial development and broadening the availability of the technologies, whether it be ground-breaking point-of-care testing, like Cellspect, or world-leading rehabilitation technology, like Cyberdyne. Our role will be to educate, inform and sometimes even train healthcare providers, so together we can accelerate uptake and make these advances more accessible to the people who can most benefit.
But this is only one model. As I mentioned, we are building a very versatile approach to opportunity development. We’ll be looking at different types of agreement, leveraging what has worked successfully for the group in the past, assessing possible partnership models, to make sure that everything we do takes us closer to our overarching aim: to make high quality healthcare accessible to as many people as possible, particularly in markets where accessibility has historically been challenging.
[1] https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(17)30488-6/fulltext
[2] https://elibrary.worldbank.org/doi/10.1596/978-1-4648-0527-1_ch13#
[3] https://www.who.int/hdp/en/
[4] ‘Modeling the effects of health on economic growth’ Journal of Health Economics, Volume 20, issue 3
[5] https://www.journals.uchicago.edu/doi/abs/10.1086/529000





 1x
1x

 Added to press kit
Added to press kit


